Project 2004
May 29 - June 6, 2004
In 2002, we began our preparations for our first project, that was to take place in 2004 in Addis Ababa, the capital of Ethiopia. We planned to implant heart valves in twenty children suffering from heart valve disease.
We had two different major tasks to consider.
For one, it was necessary to establish contacts in Addis Ababa that were willing to support and promote our project. This included the search for a suitable hospital that was able to provide our team with an operating room and accommodation for an intensive care unit. Furthermore, medical professionals in Addis Ababa were needed to screen patients for possible operative therapy and to provide long-term follow-up care for those patients who received heart valve replacements. The children with heart valve replacements must receive anti-coagulant medication for the rest of their lives. Treatment with this medication requires a life-long monitoring of the blood coagulation values by means of a laboratory test, a test which can also be performed by the patients themselves.
The contacts were established through Dr. Kifle Tondo. He is the initiator of this project, an Ethiopian, and a cardiac surgeon himself. In the Black Lion Hospital, a University Hospital in Addis Ababa, we found a very reliable and friendly partner for our cooperation. The dean of the medical faculty whole-heartedly supported our project and provided us with two competent colleagues, Dr. Kinfu (an anesthesiologist) and Dr. Gedlu (a cardiologist) . Without the help of these two colleagues, the realization of our project would not have been possible.
We had two different major tasks to consider.
For one, it was necessary to establish contacts in Addis Ababa that were willing to support and promote our project. This included the search for a suitable hospital that was able to provide our team with an operating room and accommodation for an intensive care unit. Furthermore, medical professionals in Addis Ababa were needed to screen patients for possible operative therapy and to provide long-term follow-up care for those patients who received heart valve replacements. The children with heart valve replacements must receive anti-coagulant medication for the rest of their lives. Treatment with this medication requires a life-long monitoring of the blood coagulation values by means of a laboratory test, a test which can also be performed by the patients themselves.
The contacts were established through Dr. Kifle Tondo. He is the initiator of this project, an Ethiopian, and a cardiac surgeon himself. In the Black Lion Hospital, a University Hospital in Addis Ababa, we found a very reliable and friendly partner for our cooperation. The dean of the medical faculty whole-heartedly supported our project and provided us with two competent colleagues, Dr. Kinfu (an anesthesiologist) and Dr. Gedlu (a cardiologist) . Without the help of these two colleagues, the realization of our project would not have been possible.
Our second task was to clarify what equipment and supplies as well as how much manpower were necessary for such an undertaking. We decided to travel to the Black Lion Hospital with a team consisting of four anesthesiologists, two anesthesia nursing professionals, four surgeons, two operative nursing professionals, two cardiac perfusionists, and four intensive care nursing professionals. The team was further supported by Hareg and Karingo, the wife and son of Kifle Tondo. Hareg, due to her Ethiopian origins, was an irreplaceable asset providing assistance with translations, explanations of common practices and other sorts of helpful information, and she became an integral part of our team. Furthermore, Marion Lenz, the press spokeswoman for the Braunschweig City Hospital, was responsible for the professional photo documentation of the project. Lennert Koß took part as a trainee and mastered his first trials in the medical arena with bravado.
With regard to the size of the team, we learned in our first project that more personnel was needed in the area of intensive care medicine. The team members used vacation time to take part in the project and financed the flight travel costs, as far as possible, themselves.
Twenty heart valve replacement operations with the use of a heart-lung machine and the intensive care treatment following the operations had to be planned for this project. For this purpose, not only the heart-lung machine itself, but also the ventilators, automatic injection pumps, surgical instruments, and the artificial heart valves had to be provided. All of the consumable materials from soap and disinfectants for the operating team to suction catheters, bandages and dressing materials for the intensive care unit had to be ordered, acquired, packed, and shipped.
New aspects with regard to the handling of medications that were purchased and stored in Germany and that then needed to be transported across international borders had to be considered. Special rules apply to the anesthetic medications, as they are regulated by drug laws and their use is stringently controlled.
With regard to the size of the team, we learned in our first project that more personnel was needed in the area of intensive care medicine. The team members used vacation time to take part in the project and financed the flight travel costs, as far as possible, themselves.
Twenty heart valve replacement operations with the use of a heart-lung machine and the intensive care treatment following the operations had to be planned for this project. For this purpose, not only the heart-lung machine itself, but also the ventilators, automatic injection pumps, surgical instruments, and the artificial heart valves had to be provided. All of the consumable materials from soap and disinfectants for the operating team to suction catheters, bandages and dressing materials for the intensive care unit had to be ordered, acquired, packed, and shipped.
New aspects with regard to the handling of medications that were purchased and stored in Germany and that then needed to be transported across international borders had to be considered. Special rules apply to the anesthetic medications, as they are regulated by drug laws and their use is stringently controlled.
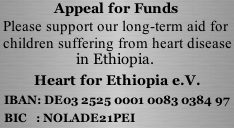
Furthermore, it was necessary to obtain international working permits for all team members, to organize the required vaccination protection prior to the project start, to understand and meet customs regulations for the export and import of the necessary project materials, and most importantly to request donations and to organize donation drives to raise the money needed to fund this undertaking. It would be impossible to list all of the organizational activities behind such a project here. Suffice it to say that everything was carried out in a timely and successful manner. We found interested and supportive people in many organizations, government offices, and companies whose essential contributions allowed this project to become a reality. Here we would like to express our heartfelt thanks to all parties for the help and support they provided in bringing a seemingly impossible proposal to a successful completion.
The flight from Frankfurt, Germany, to Addis Ababa, Ethiopia, departed on May 29, 2004. Upon arrival in Addis Ababa, we were driven to the pre-arranged accommodations supplied by the International Red Cross. Afterward there was a welcoming reception hosted by the dean of the University of Addis Ababa where we were introduced to the local medical and nursing colleagues. For many of us, this was the first contact with the African continent and its people, and it was a very emotionally moving moment, that will remain unforgettable.
Now we were ready to begin our work. To our great relief, all the transported materials had arrived undamaged and had already been seen and sorted out by Cornelia Schollbach and Dr. Tondo, who had traveled to Ethiopia a few days earlier.
Three groups were formed with different tasks:
A great deal of flexibility and creativity was needed in order to reconcile the expectations and requirements of our highly technological medicine with the reality of the Ethiopian conditions. In a joint effort, all of the obstacles, large or small, were mastered, albeit sometimes in quite unconventional, but functional, ways. It was interesting to observe that the team members strived to achieve a certain German orderliness.
Now we were ready to begin our work. To our great relief, all the transported materials had arrived undamaged and had already been seen and sorted out by Cornelia Schollbach and Dr. Tondo, who had traveled to Ethiopia a few days earlier.
Three groups were formed with different tasks:
- Setting up of the operating room including the heart-lung machine;
- Organizing the intensive care unit (ICU);
- Selection of the children to be treated.
A great deal of flexibility and creativity was needed in order to reconcile the expectations and requirements of our highly technological medicine with the reality of the Ethiopian conditions. In a joint effort, all of the obstacles, large or small, were mastered, albeit sometimes in quite unconventional, but functional, ways. It was interesting to observe that the team members strived to achieve a certain German orderliness.
The doctors in the team met with Dr. Kinfu and Dr. Gedlu. The Ethiopian doctors presented the cases of these sick children, and together the doctors reviewed the medical data and re-examined the patients. The children came with their entire families from remote areas of the country, some had traveled long distances by foot. At the end of this patient review, the patient selection and operation schedules were completed.
The team met the evening before the first operation and finalized the preparations for the following day. With great expectations and a certain degree of tension, we all arrived in the operating tract the next morning. The thoughts and emotions of Tekeste Amka, though, must have been indescribable, as he was confronted with us and our modern western medical technology in his homeland. This 15-year-old boy suffered from defective heart valves between the left atrium and the left ventricle (mitral valve insufficiency) and between the right atrium and right ventricle (tricuspid valve insufficiency). Both heart valves were successfully reconstructed.
During the induction of the anesthesia, the tension lessened as we began to perform our routine professional procedures, and remarkable work was accomplished under unusual African conditions.
During the induction of the anesthesia, the tension lessened as we began to perform our routine professional procedures, and remarkable work was accomplished under unusual African conditions.
We would like to underscore that the publication of the name and diagnosis of our first patient occurred with the express consent of the patient and his family.
In the next two weeks, nineteen further operations were performed. The mean age of the patients was 14.4 years of age, and we operated on twelve girls and eight boys. In total, ten mitral valves (heart valve between the left atrium and left ventricle) were replaced with a mechanical valve in combination with the reduction of the left atrium size (left atrial reduction plasty). Furthermore we performed an aortic valve replacement (heart valve between the left ventricle and the aorta) in two patients, and in six patients both the mitral valve and the aortic valve were successfully replaced.
Our team implanted a pacemaker in one 8-year-old boy, and in an 18-year-old patient a portion of the heart muscle in the left ventricle was removed because an asymmetric thickening caused a reduction in blood flow out of the left ventricle (myotomy/myectomy). All of the patients, which we refer to now as “our children”, were treated in the intensive care unit after the operation. Here we becane acquainted with the families of our patients and gained profound insight into the Ethiopian lifestyle. This was an intensely emotional time in the lives of “our children”, their families, and our team members. Impressions of this experience in the form of photographs can be viewed on this website under media.
Our team implanted a pacemaker in one 8-year-old boy, and in an 18-year-old patient a portion of the heart muscle in the left ventricle was removed because an asymmetric thickening caused a reduction in blood flow out of the left ventricle (myotomy/myectomy). All of the patients, which we refer to now as “our children”, were treated in the intensive care unit after the operation. Here we becane acquainted with the families of our patients and gained profound insight into the Ethiopian lifestyle. This was an intensely emotional time in the lives of “our children”, their families, and our team members. Impressions of this experience in the form of photographs can be viewed on this website under media.
We would like to underscore here two important factors that were decisive in the achievement of our goals:
- The success of the operations was only possible because of the warm welcome and sincere acceptance given to us by the Black Lion Hospital in Addis Ababa and due to the cooperation and support of many medical staff doctors and nurses there;
- The adaptation of our team members to the, for our middle European medical mentality, extremely unusual conditions bound our team members together.